- Category
- …
- Category
- Category
- …
- Category
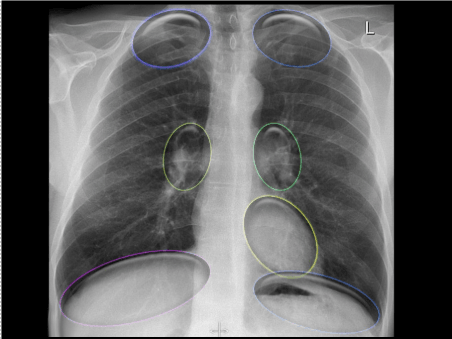
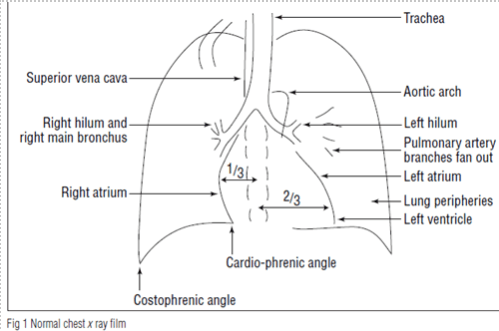
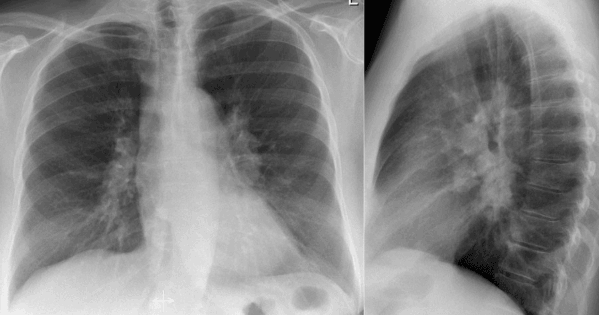
Normal Chest Xray
WHICH TISSUE DENSITIES CAN WE SEE ON THE RADIOGRAPH?
In order of increasing density, they are:
air – lungs
fat – in breast & subcutaneous tissues, & around muscle
water (soft tissue) – heart, muscle, blood
metal or Ca++ - bone, metallic hardware, contrast agents
On the radiograph, anatomic structures are recognized by their different densities and by their different abilities to absorb or attenuate the X-ray beam
FILM EXPOSURE:
- Traditional radiography has been performed with film-screen cassettes.
- Direct radiography (DR) is a group of technologies that can indirectly or directly convert X-ray intensity into electric signals.
- Simplistically, when the radiographic film is exposed to radiation, the silver ion in its emulsion precipitates.
- What color is silver ion?? It is BLACK.
- An area of film exposed to more radiation will be blacker than an area that receives less.
- In the chest
* Air density is low-->allow the silver ions to go through-->more ions will precipitate on film-->appear black
* Bone density is high--> block(absorb) the silver ions--> fewer ions will precipitate on film-->appear white
With an optimally exposed image, the disc spaces of the spine are barely perceptible through the heart.
- When we accidentally over-expose (over-penetrate) an image, it receives excess radiation, and all structures will appear too black.
- In contrast, when we use insufficient exposure or when a patient is obese, the image is under-exposed (under-penetrated). The image then receives too little radiation, very little silver ion is deposited, and all structures will be too white.
over-exposed = too black
under-exposed = too white
- Both over- and under-exposure limit the detection of pathology.
THE SILHOUETTE SIGN:
- The silhouette sign helps us identify and localize pathology, especially in the thorax.
- The silhouette sign is the normal interface between two structures of different densities
air in the lungs and soft tissue of the heart
- It is the loss of a normal silhouette that indicates pathology.
- Normally, when two substances of water density are in anatomic contact, they cannot be differentiated from each other, and their interfaces cannot be perceived.
- Blood within the lumen of the heart cannot be distinguished from contiguous heart muscle.
- Both look “white” on radiography.
- However, when the lung (air density) is filled in with pneumonia (water density)-->the normal air-water interface between the lung and the adjacent heart border will be obscured.
- Thus, the heart border is obliterated or “silhouetted” by the pneumonia.
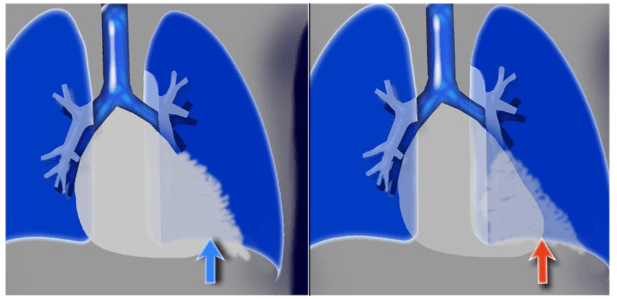
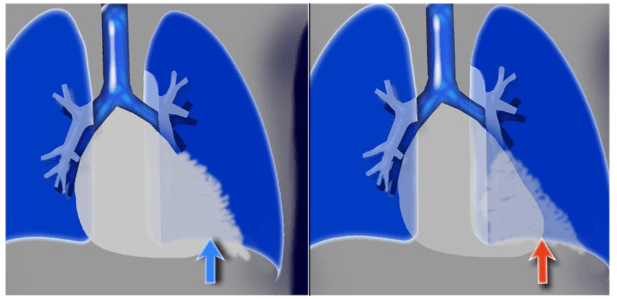
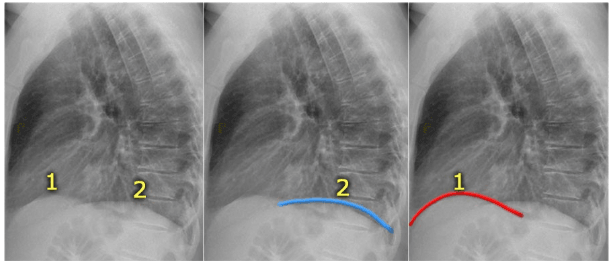
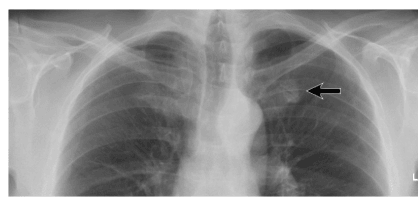
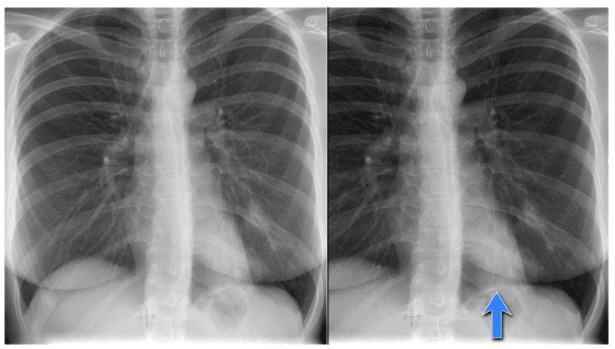
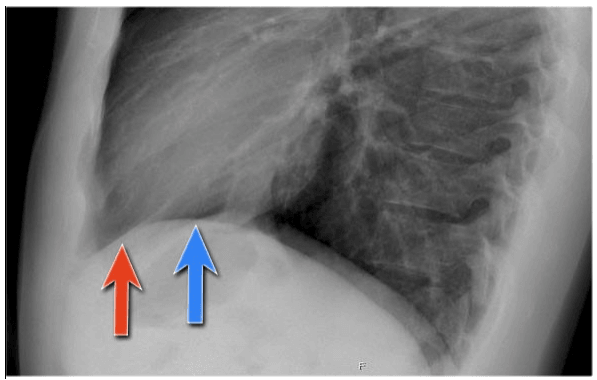
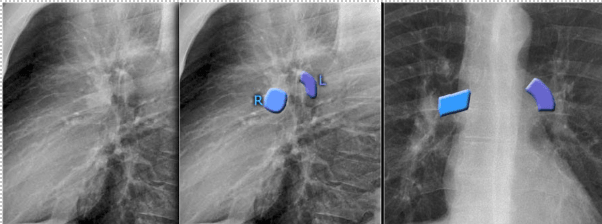
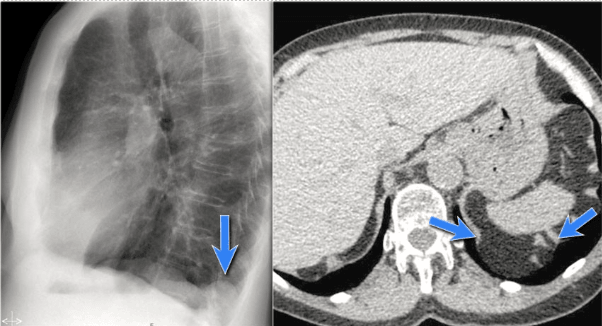
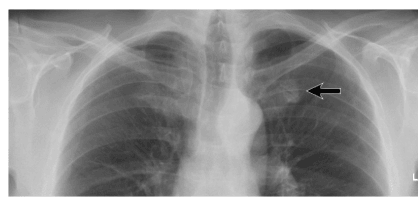
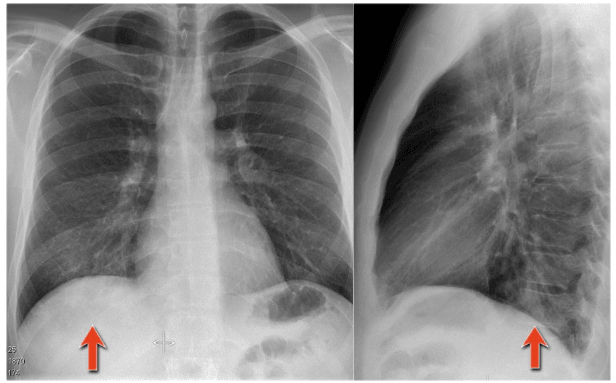
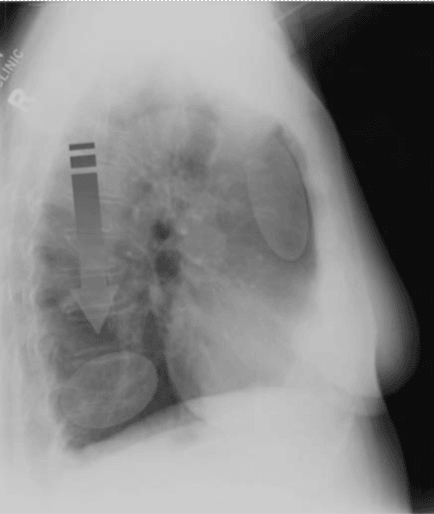
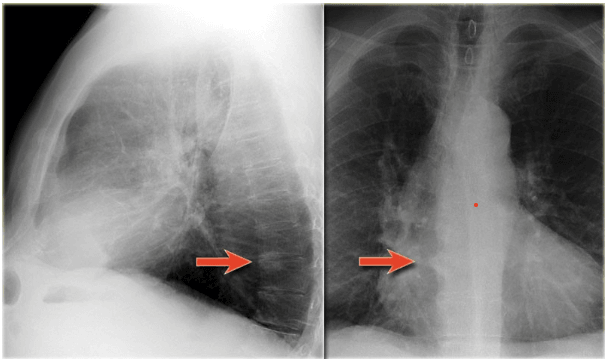
- The heart is located anteriorly in the chest and it is bordered by the lingula of the left lung. The difference in density between the heart and the air in the lung enables us to see the silhouette of the left ventricle. When there is something in the lingula with the same 'water density' as the heart, the normal silhouette will be lost (blue arrow).
- When there is a pneumonia in the left lower lobe, which is located more posteriorly in the chest, the left ventricle will still be bordered by air in the lingula, and we will still see the silhouette of the heart (red arrow).
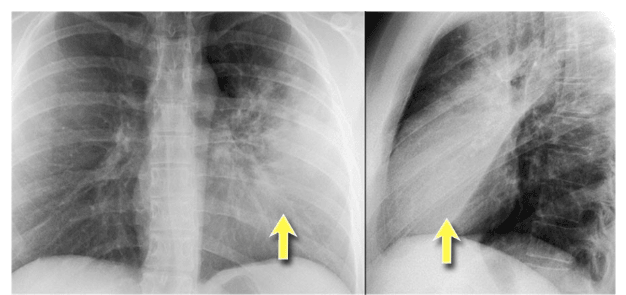
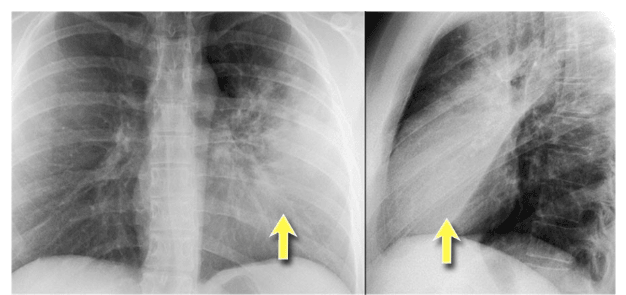
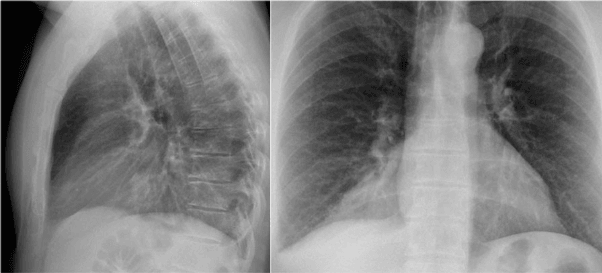
- The PA-film shows a silhouette sign of the left heart border.
Even without looking at the lateral film, we know, that the pathology must be located anteriorly in the left lung.
This was a consolidation due to a pneumonia.
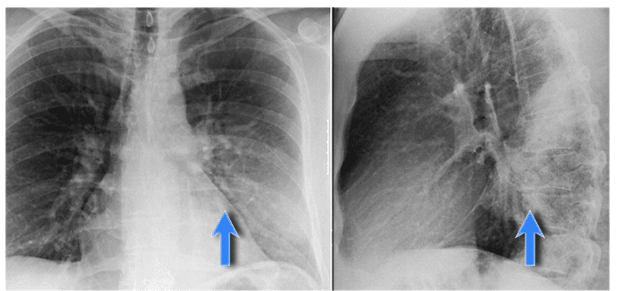
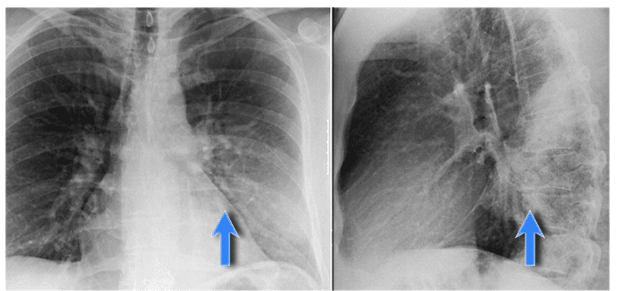
- Here we see a consolidation which is located in the left lower lobe.
There is a normal silhouette of the left heart border.
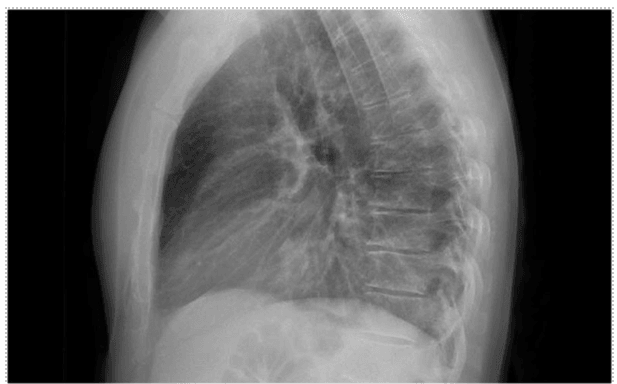
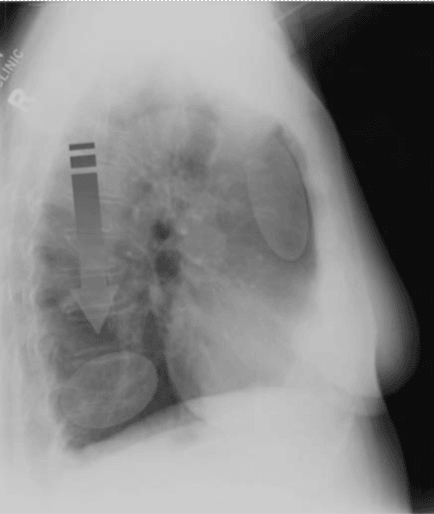
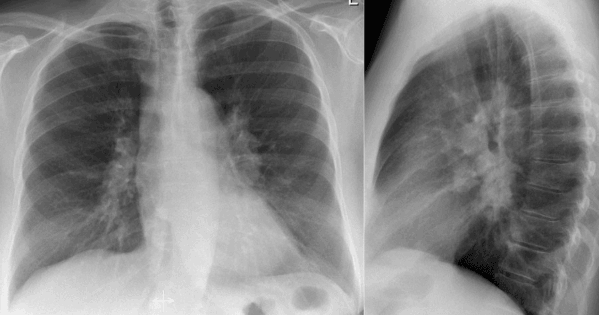
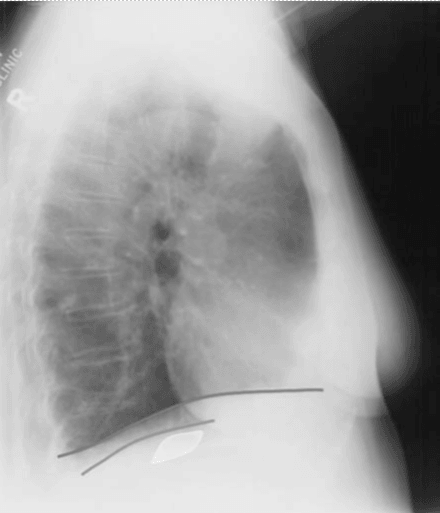
- On this lateral film there is too much density over the lower part of the spine.
- By only looking at the interfaces of the left and right diaphragm on the lateral film, it is possible to tell on which side the pathology is located.
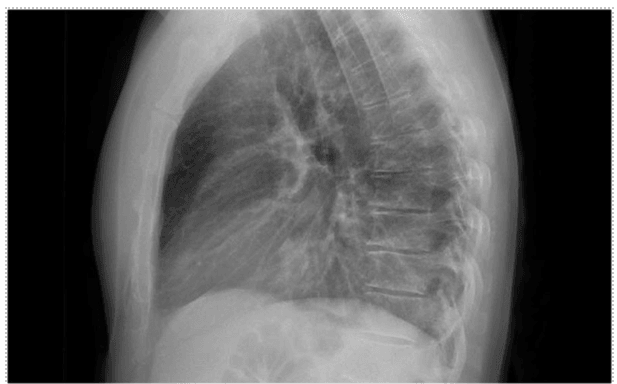
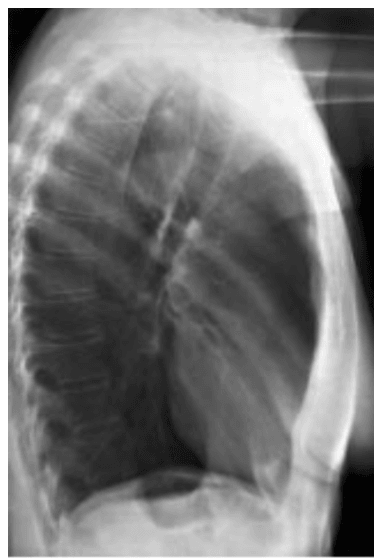
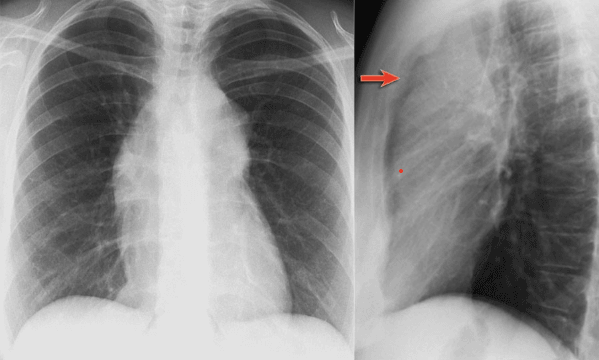
- First study the lateral film.
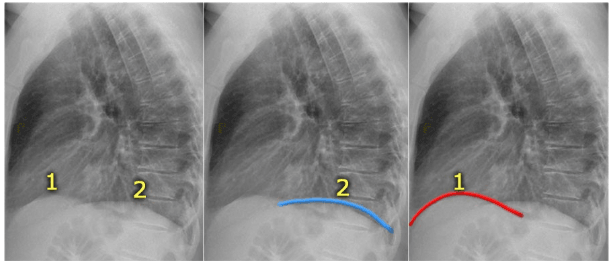
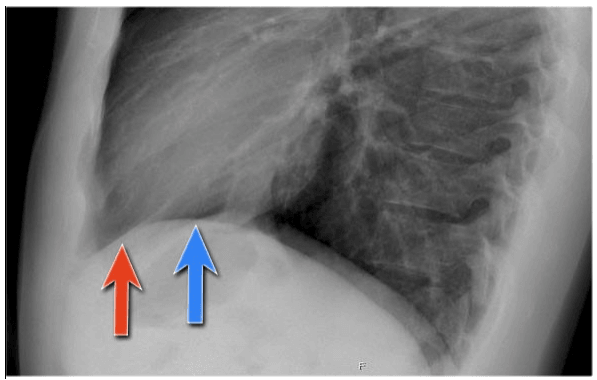
- On a normal lateral chest film the silhouette of the left diaphragm 2- can be seen from posterior up to where it is bordered by the heart, which has the same density (blue arrow).
- One should be able to follow the contour of the right diaphragm -1- from posterior all the way to anterior, because it is only bordered by the lung.
- Here we cannot follow the contour of the right diaphragm all the way to posterior, which indicates that there is something of water-density in the right lower lobe (red arrow).
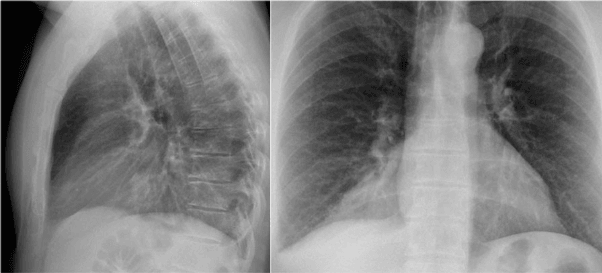
- On the PA-film there is a normal silhouette of the heart border, so the pathology is not in the anterior part of the chest, which we already suspected by studying the lateral view.
- Why do we still see the silhouette of the right diaphragm on the PA-film?
- What we see is actually the highest point of the right diaphragm, which is anterior to the pneumonia in the right lower lobe.
The pneumonia does not border the highest point of the diaphragm.
HOW TO DISPLAY THE CHEST RADIOGRAPH?
- We display the PA or AP as if we are facing the patient.
- The patient’s right is on our left, and his left is on our right. The films will be labeled with side.
- We place the lateral CXR as if the patient is facing towards our left.
STANDARD RADIOGRAPHIC VIEWS:
A FUNDAMENTAL rule of radiology is to put the area of interest as close as possible to the image cassette.
1. The Postero-Anterior (PA) radiograph:
- Most CXRs are taken in a PA position
- The term PA refers to the direction of the X-ray beam, which horizontally traverses the patient from posterior to anterior.
- The patient stands in front of the x-ray film cassette with their chest against the cassette and their back to the radiographer.
- The X-ray beam passes through the patient from back to front (i.e. PA) onto the film.
- The patient’s anterior chest wall is placed next to the film cassette. (Why? Because the heart is an anterior structure, placing the heart next to the cassette reduces MAGNIFICATION and increases image SHARPNESS.)
- Heart and mediastinum are thus closest to the film
- This view is taken during deep inspiration with the patient upright and 6 feet from the X-ray tube.
- PA is preferred when possible because:
- It’s quicker
- Inspiration is improved
- Heart is less magnified
- Special considerations in PA film:
- It is important to examine all the areas where the lung borders the diaphragm, the heart, and other mediastinal structures.
- At these borders, lung-soft tissue interfaces are seen resulting in either:
- Line or stripe:
- right para tracheal stripe
- paraspinal line
- para-aortic
- azygoesophageal line or recess
- Vena azygos lobe
2. Silhouette:
- for instance the normal silhouette of the aortic knob or left ventricle
- The anterior and posterior junction lines are formed where the upper lobes join anteriorly and posteriorly. These are usually not well seen

2. The Antero-Posterior (AP) radiograph
- Substituted for the PA when the patient is unable to stand or sit.
- In this instance, the patient’s back is placed against the film cassette, and the X-ray beam traverses the patient from anterior => to posterior.
- When a patient is unable to be moved, an AP radiograph may be performed with portable equipment.
- Special considerations in AP film:
- Because of low ceilings and portable equipment, the AP is usually taken at a distance of 3 feet. Compared to the PA, this increases magnification and decreases image sharpness.
- heart and mediastinum are distant from the cassette and are therefore subject to x-ray magnification.
- As a result it is very difficult to make an accurate assessment of the cardio mediastinal contour on an AP film.
- Neonatal xrays are always AP so, remember to look for the thymus:
3. The other routine view is the Left Lateral CXR (LL CXR).
- The left side of the chest is placed against the film cassette, and the X-ray beam traverses the patient from right to left.
- We perform a LEFT LATERAL CXR rather than a right lateral because
- the heart is on the left. This places the heart as close as possible to the film cassette, thus decreasing cardiac magnification and increasing sharpness.
- The LL CXR also gives a better look at the lung (left lower lobe) behind the heart.


CXR APPROACH PATTERN:
- Identity:
- Name, date, gender, date of study.
- Errors do occur and those relating to labelling of the radiograph are the most common.
2. Technical: (C-A-F-E)
C = centralized/rotated.
- First, assess patient's position
- The spinous processes of the thoracic vertebrae should be midway between the medial ends of the clavicles.
- Length of anterior ribs showed to be equal on both sides.
- The anterior ribs should be equidistant from the lateral margins of the spine and posterior spinous processes of the vertebra.
- the lateral view, there should be a very small distance between the posterior right and left rib margins.
* Slight rotation to the left--> enlargement of the left superior mediastinum and left cardiac structures.
* Slight rotation to the right--> enlargement of the mediastinal and cardiac structures
- A lordotic image can exaggerate the size of the cardiac apex
- If the patient is rotated, it can be either to the left or to the right.
The rotation can be assessed by:
- Measuring the distance between the spinous process and the medial ends of one of the ribs
* If unequal (one side shorter than the other) --> the patient is rotated
2. Comparing the densities of the two hemi-thoraces
* The side with the darker(more black) hemithorax--> is the side to which the patient is rotated
(irrespective of whether the CXR has been taken PA or AP)


A = AP or PA view:
PA
- You can see the stomach bubble and the apices of the lungs above the clavicles.
- The mediastinum appears normal.
AP
- You cannot see the stomach bubble and the apices of the lungs above the clavicles.
- An anterior-posterior film will always be labeled as AP, so if nothing is written on the film it is safe to assume it is PA.
F = Film inspiratory/expiratory
In the Inspiratory film:
- Count: 7 complete anterior ribs or 9 posterior ribs are visible. If more than six anterior ribs imply hyper-expanded lungs.
- A good inspiratory image is one in which the anterior sixth or posterior eighth rib is visualized above the apex of the left hemidiaphragm.
- The lower third of the heart is visible above the diaphragm.
- Diaphragms: should lie at the level of the sixth ribs anteriorly. The right hemidiaphragm is usually higher than the left because the liver pushes it up.
In the expiratory film:
- less than 7 complete anterior ribs or 9 posterior ribs are visible.
- the lower third of the heart is visible below the diaphragm.
Several potentially false findings can result from assessing films with poor expansion:
- Apparent cardiomegaly
- Apparent hilar abnormalities
- Apparent mediastinal contour abnormalities
- Lung parenchyma tends to appear of increased density, i.e. ‘white lung'.



E = exposure under/over:
- On a high-quality radiograph, the vertebral bodies should just be visible through the heart.
- If the vertebral bodies are not visible, then an insufficient number of X-ray photons have passed through the patient to reach the x-ray film (underexposure)-->as a result, the film will look ‘whiter’ leading to potential ‘overcalling’ of pathology.
- Similarly, if the film appears too ‘black’, then too many photons have resulted in (overexposure) of the x-ray film-->this ‘blackness’ results in pathology being less conspicuous and may lead to ‘undercalling’.
Underexposure --> ‘whiter’ --> ‘overcalling’ of pathology
Overexposure --> ‘blacker’ --> ‘undercalling’ of pathology

3. Anatomical:
The trachea
- The trachea lies in the mediastinum and is displaced slightly to the right by the left-sided aortic arch (mainly the lower third of the trachea) but can be pathologically pushed or pulled to either side, providing indirect support for an underlying abnormality
- It divides at the carina (T4-6) into the L & R main bronchi, which continue into the lung.
The left main bronchus
- It is longer (5 cm), inferior, and more horizontal than the right.
- Divides into LUL and LLL bronchi.
The right main bronchus
- It is shorter (2.5 cm) and more superior and vertical.
- Divides into the RUL and bronchus intermedius, which then divides into RML & RLL bronchi.
- Smaller bronchi are not normally detected in the lung unless diseased.
Para-tracheal stripe
- The right wall of the trachea should be clearly seen as the so-called right para-tracheal stripe.
- The para-tracheal stripe is visible by quality of the silhouette sign: air within the tracheal lumen and adjacent right lung apex outline the soft-tissue-density tracheal wall.
- Loss or thickening of the para-tracheal stripe intimates adjacent pathology.
- Widening of the paratracheal line (> 2-3mm) may be due to
- Lymphadenopathy
- Pleural thickening
- Hemorrhage
- Fluid overload and heart failure

The aortic arch
- Is the first structure on the left, followed by the left pulmonary artery; then you can trace the pulmonary artery branches fanning out through the lung.
- Dilation of the trachea is obvious on the plain radiograph, with the tracheal shadow often being as wide as the vertebral bodies.
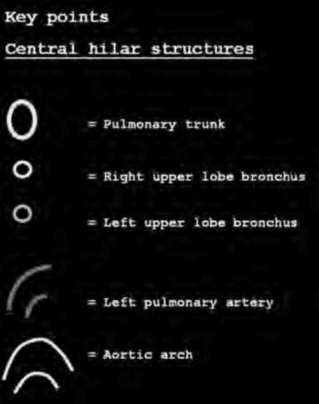
The hilar regions
- The hila are where the pulmonary arteries and veins and main bronchi enter the lung.
- The normal hilar shadow is 99% composed of vessels - pulmonary arteries and to a lesser extent veins
- Both hilar should be of similar density and concave.

- The vessel margins are smooth and the vessels have branches.
- The left hilum is superior to the right in 98% of normal CXRs.
- The right and left hila have the same height in 2% of normal CXRs.
- The right hilum is NEVER normally higher than the left.
- The left hilum is usually superior to the right by up to 1 cm.

- This results from the superior pulmonary vein crossing the lower lobe pulmonary artery.
- The point of intersection is known as the hilar point (HP).
- The pulmonary arteries (PA’s) parallel the bronchi. They are vertically oriented and divide into upper and lower branches.
- The right pulmonary artery (RPA) passes in front of the bronchi.
- The left pulmonary artery (LPA) arches over the L main bronchus and is more superiorly oriented than the RPA.
- The pulmonary veins are more horizontal than the PA’s and do not parallel the bronchi. They form a single trunk from each lobe of the lung and drain into the left atrium. The inferior pulmonary veins form the lowest part of the hila.

- In this illustration the lower lobe arteries are coloured blue because they contain oxygen-poor blood.
- They have a more vertical orientation, while the pulmonary veins run more horizontally towards the left atrium, which is located below the level of the main pulmonary arteries.

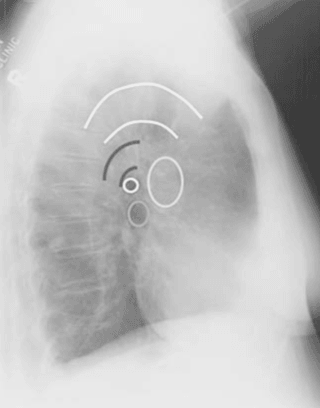
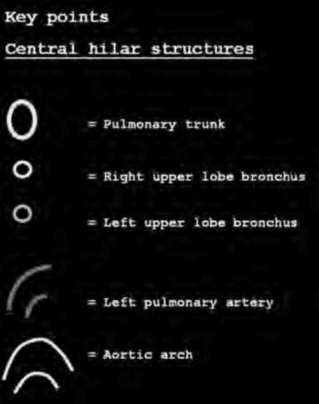
- Both pulmonary arteries and veins can be identified on a lateral view and should not be mistaken for lymphadenopathy.
- Sometimes the pulmonary veins can be very prominent.
- The left main pulmonary artery passes over the left main bronchus and is higher than the right pulmonary artery which passes in front of the right main bronchus.
- These images are thick slab sagittal reconstructions of a chest-ct to get a better view of the hilar structures.

- The lower lobe pulmonary arteries extend inferiorly from the hilum.
They are described as little fingers because each is the size of a little finger. - On the right side, the little finger will be visible in 94% of normal CXRs and on the left side in 62% of normals.
Normal hili are:
- Normal in position - left higher than right
- Equal density
- Normal branching vessels
Enlarged hilar area (bulky):

- Enlargement of the hili is usually due to lymphadenopathy or enlarged vessels.

- In this case there is an enlarged hilar shadow on both sides. This could be the result of enlarged vessels or enlarged lymph nodes. A very helpful finding in this case is the mass on the right of the trachea.
- This is known as the 1-2-3 sign in sarcoidosis, i.e. enlargement of left hilum, right hilum and paratracheal.
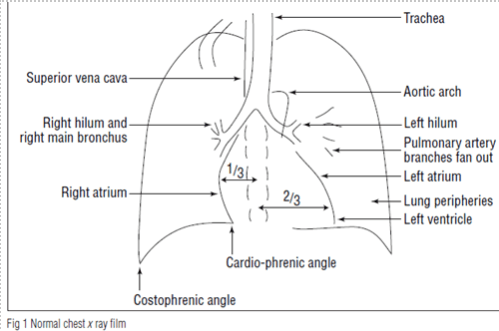
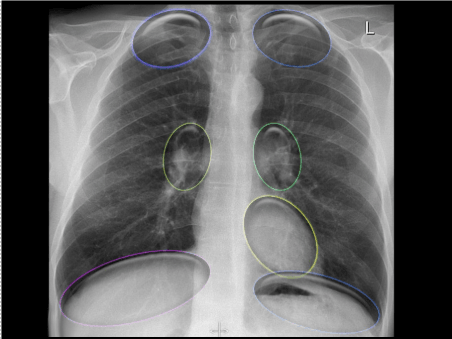
Heart and mediastinum
Assessment of heart size
- Two thirds of the heart lies on the left side of the chest, with one third on the right
- The heart size is normally less than half the widest diameter of the thorax
- The cardiothoracic ratio should be less than 0.5. i.e. A/B < 0.
- A cardiothoracic ratio of greater than 0.5 (in a good quality film) suggests cardiomegaly.
- in neonates < 0.6

Assessment of cardiomediastinal contour

Special consedirations:
- Mediastinal lines or stripes are interfaces between the soft tissue of mediastinal structures and the lung
- Displacement of these lines is helpful in finding mediastinal pathology

1) The paraspinal line: may be displaced by a
- Paravertebral abscess
- Hemorrhage due to a fracture
- Extravertebral extension of a neoplasm
2) Para-aortic line: Displacement of the para-aortic line can be due to
- Elongation of the aorta
- Aneurysm
- Dissection
- Rupture
3) The azygoesophageal recess
- An important mediastinal-lung interface to look for is the azygoesophageal line or recess, the most important mediastinal line to look for
- The azygoesophageal recess is the region inferior to the level of the azygos vein arch in which the right lung forms an interface with the mediastinum between the heart anteriorly and vertebral column posteriorly, it is bordered on the left by the esophagus.

- Deviation of the azygoesophageal line is caused by (SBAHE):
- Subcarinal lymphadenopathy
- Bronchogenic cyst
- Atrial (Left) enlargement, mitral stenosis
- Hiatal hernia
- Esophageal disease (dilatation/achalasia, carcinoma)

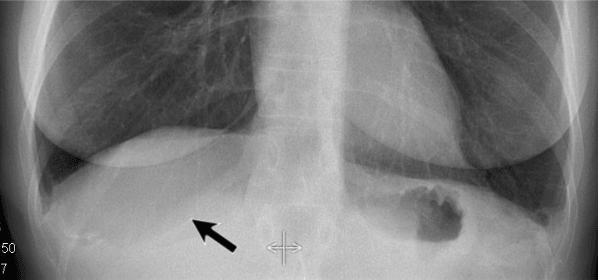
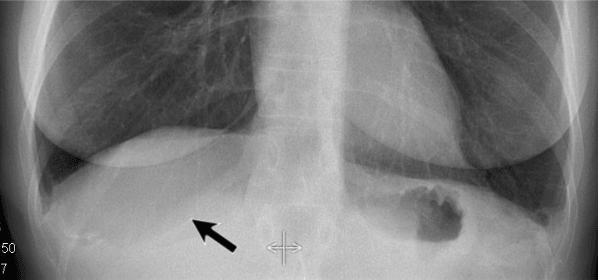
- Notice the deviation of the azygoesophageal line on the PA-film
- Caused by a hiatal hernia

- A hiatal hernia is the most common cause of displacement of the azygoesophageal line
- Notice the air within the hernia on the lateral view

- Another common cause of displacement of the azygoesophageal line is subcarinal lymphadenopathy
- Notice the displacement of the upper part of the azygoesophageal line on the chest x-ray in the area below the carina
This is the result of massive lymphadenopathy in the subcarinal region - There are also nodes on the right of the trachea displacing the right paratracheal line

- There is displacement of the azygoesophageal line both superiorly an inferiorly
- There is an air-fluid level (arrow)
Combined with the above this must be a dilated esophagus with residual fluid. The final diagnosis was achalasia - The density on the left in the region of the lingula is the result from prior aspiration pneumonia

- The AP-film shows a right paratracheal mass
The azygoesophageal recess is not identified, because it is displaced and parallels the border of the right atrium
The large round density in the left lung is the result of aspiration - Notice the massive dilatation of the esophagus on the CT
4) Aortopulmonary window
- The aortopulmonary window is the interface below the aorta and above the pulmonary trunk and is concave or straight laterally.
- AP-window can be convex laterally due to a mass that fills the retrosternal space
Assessment of mediastinal compartments
It is useful to consider the contents of the mediastinum as belonging to three compartments:
- Anterior mediastinum: anterior to the pericardium and trachea
- Middle mediastinum: between the anterior and posterior mediastinum
- Posterior mediastinum: posterior to the pericardial surface


Each compartment, has it's own pathology

* The thymus shrinks with
- Sepsis
- Sickness
- Steroids
Anatomy of Lungs and pleura:
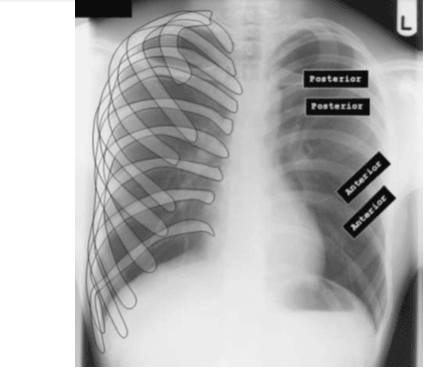
Lobar anatomy
- Three lobes in the right lung (RUL) (RML) (RLL)
- Two in the left (LUL) (LLL)
- The left lobe also contains the lingula:
- Functionally a separate ‘lobe'
- Anatomically part of the upper lobe
Pleura:
- The pleura is normally 1mm thin
- There are two layers of pleura:
- The parietal pleura lines the diaphragms, chest wall, and mediastinum
- The visceral pleura covers the lobes of the lung
- Both of these layers come together to form reflections that separate the individual lobes
- These pleural reflections are known as fissures
- The fissures are seen as a pencil thin line when tangent to the X-ray beam

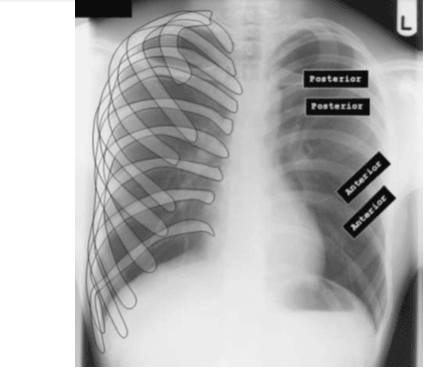
- On the right there is an oblique and horizontal fissure; the right upper lobe sits above the horizontal
fissure (HF), the right lower lobe behind the oblique fissure (OF) and the middle lobe between the
two
- On the left, an oblique fissure separates the upper and lower lobes
- Lung zones:
Upper zone at the level of rib 1 +2
Middle zone at the level of rib 3+4
Lower zone at the level of rib 5+6
- It takes about 200-300 ml of fluid before it comes visible on an CXR About 5 liters of pleural fluid are present when there is total opacification of the hemithorax.

Special consideration:
- Vena azygos lobe: A common normal variant is the azygos lobe

- The azygos lobe is created when a laterally displaced azygos vein makes a deep fissure in the upper part of the lung
- On a chest film it is seen as a fine line that crosses the apex of the right lung

- Here another patient with an azygos lobe.
The azygos vein is seen as a thick structure within the azygos fissure
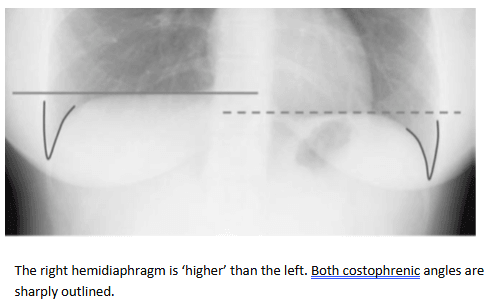
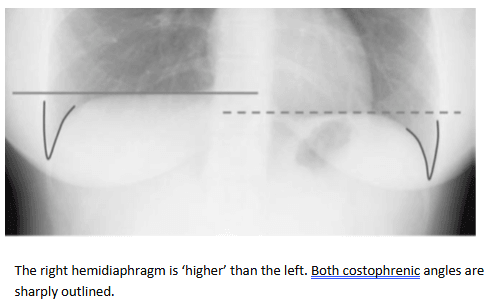
Diaphragms
- The highest point of the right diaphragm is usually 1–1.5 cm higher than that of the left.
- In 3% of cases, the left is higher but only by 1 cm. A scalloped contour is common.
- Each costophrenic angle should be sharply outlined.
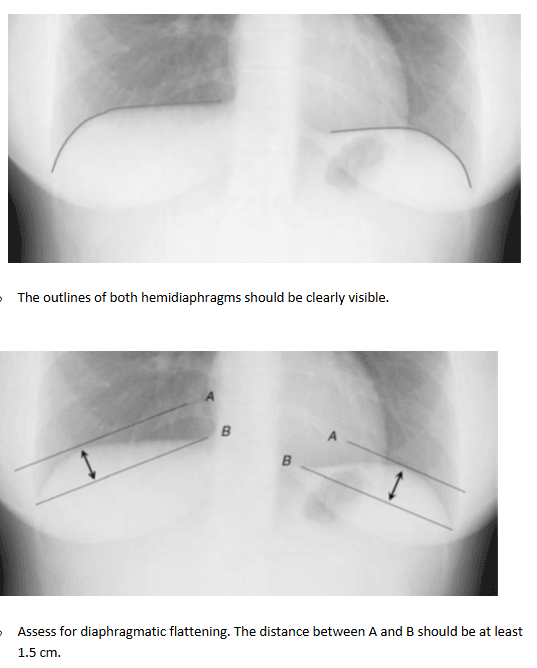
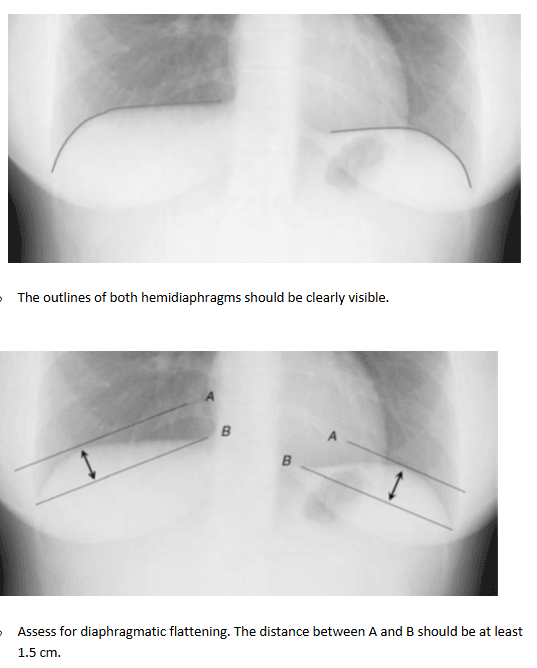
- The outlines of both hemidiaphragms should be sharp and clearly visible along their entire length (except the medial most aspect of the left hemidiaphragm).
- The ‘curvature' of both hemidiaphragms should be assessed to identify diaphragmatic flattening.
- The highest point of a hemidiaphragm should be at least 1.5 cm above a line drawn from the cardiophrenic to the costophrenic angle.
Bones and soft tissues
- It is important to examine
- every rib (from the anterior to posterior)
- the clavicles
- vertebrae
- Shoulder joints (if they are on the film).
- Similarly, look carefully at the soft tissues for asymmetry; a typical finding in cases following mastectomy (adults).
- It can be surprisingly difficult to ‘see' objects that are missing. If the ‘bones and soft tissues' are not given their due consideration, then vital information may not be appreciated.
- Remember to follow every rib, (from the anterior to posterior), the clavicles vetebrae and the shoulders.
- Special consideration:
- In some patients, an extra joint is seen in the anterior part of the first rib at the point where the bone meets the calcified cartilaginous part (arrow).
- This may simulate a lung mass.
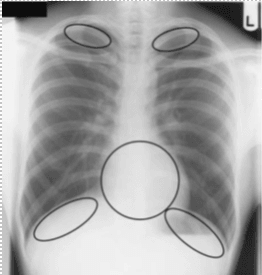
look for pathology in the ‘hidden areas:
- Some areas need special attention, because pathology in these areas can easily be overlooked:
- apical zones
- hilar zones
- retrocardial zone
- zone below the dome of the diaphragm (free air, dilated bowel, abnormal calcification, and masses)
These areas are also known as the hidden areas.
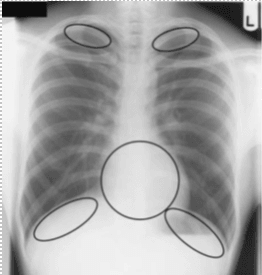
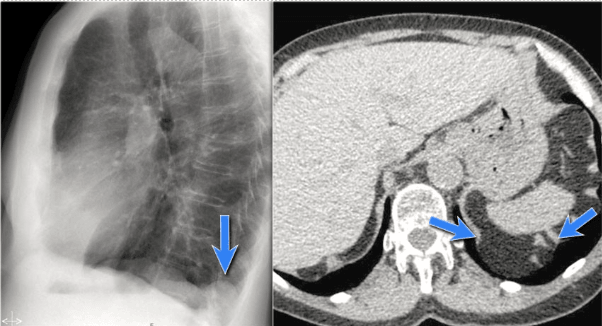
- Notice that there is quite some lung volume below the dome of the diaphragm, which will need your attention (arrow).
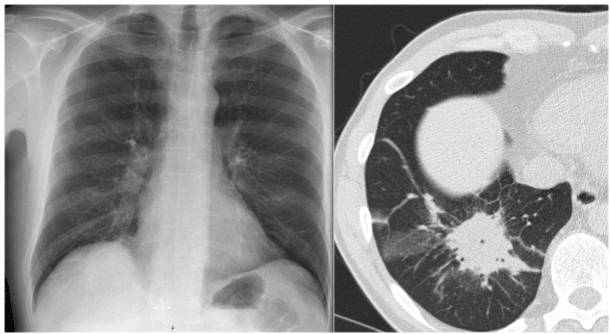
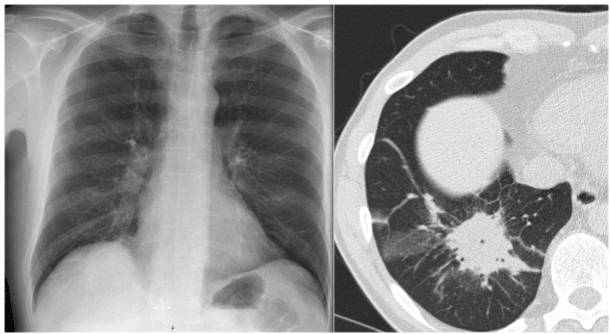
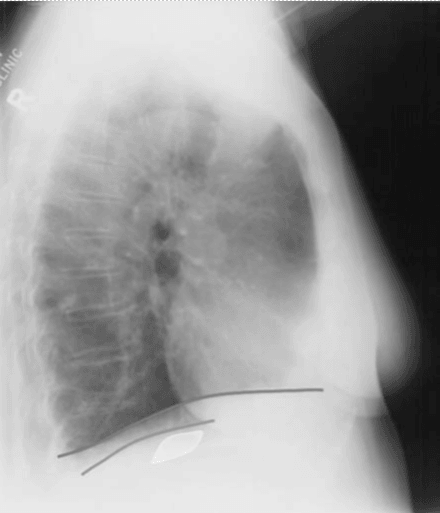
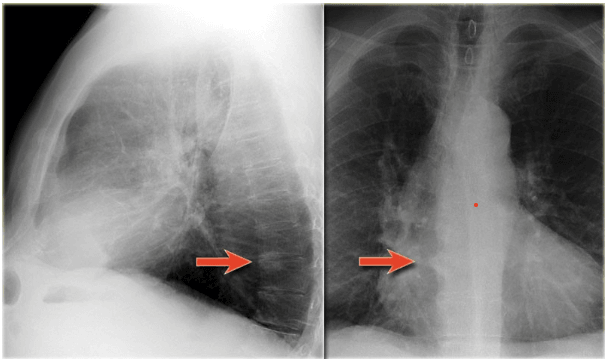
- Here an example of a large lesion in the right lower lobe, which is difficult to detect on the PA-film, unless when you give special attention to the hidden areas.
- Click on the image for an enlarged view.
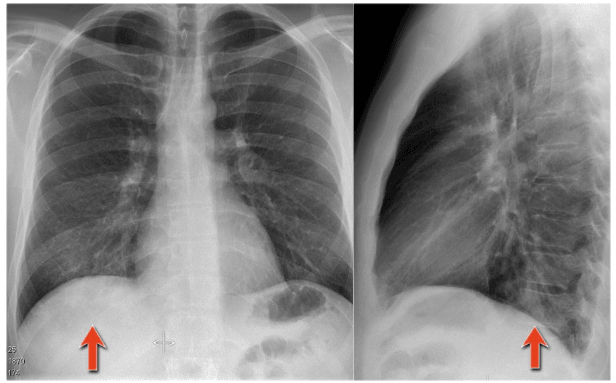
- Here a pneumonia which was hidden in the right lower lobe mainly below the level of the dome of the diaphragm (red arrow).
- Notice the increase in density on the lateral film in the lower vertebral region.
- You may have to enlarge the image to get a better view.
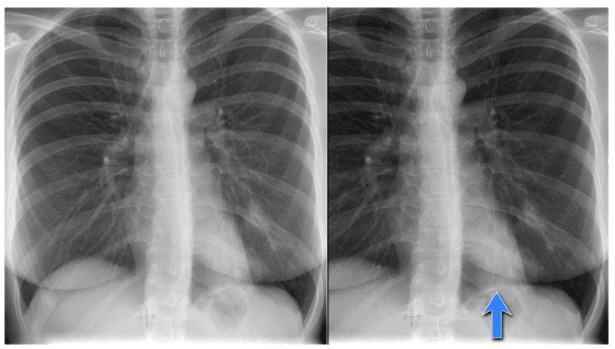
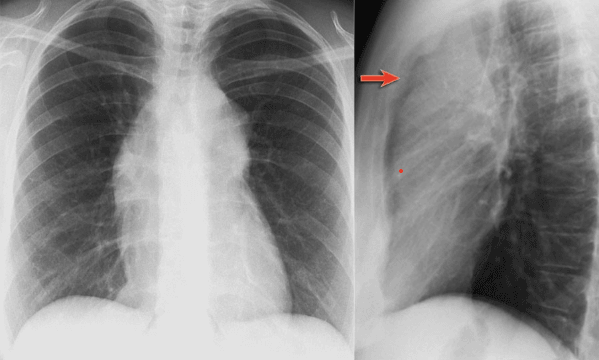
- Notice the subtle increased density in the area behind the heart that needs special attention (blue arrow).
This was a lower lobe pneumonia. - There is a subtle consolidation in the left lower lobe in the hidden area behind the heart.
Again there is increased density over the lower vertrebral region.
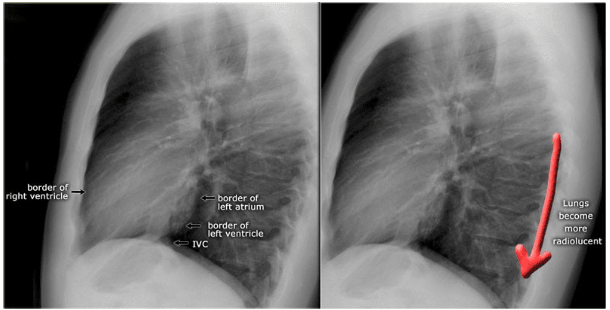
Important anatomy relating to the lateral CXR
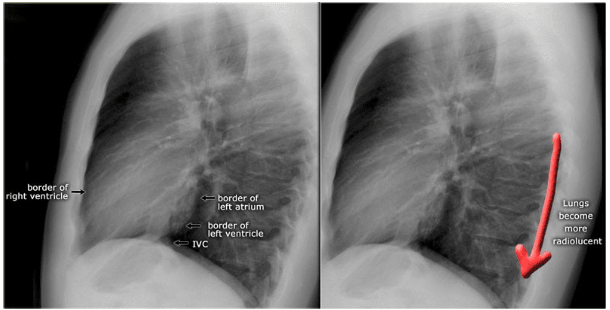
- There should be a decrease in density from superior to inferior in the posterior mediastinum as the airspaces are more in lower lobes so they should be more blackish.
- The retrosternal airspace should be of the same density as the retrocardiac airspace.
Diaphragm
- The right hemidiaphragm is usually ‘higher’ than the left.
- The outline of the right can be seen extending from the posterior to anterior chest wall.
- The outline of the left hemidiaphragm stops at the posterior heart border. Air in the gastric fundus is seen below the left hemidiaphragm
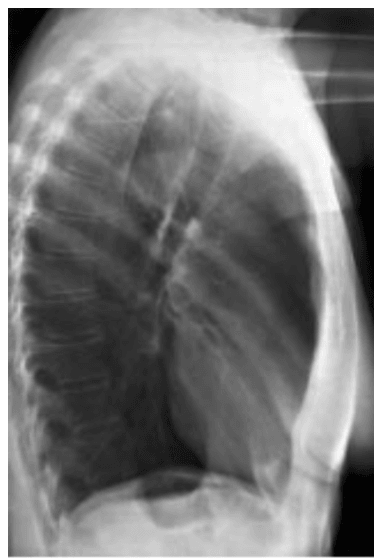
- There are only two spaces to look at on the lateral film.
- The heart lies antero-inferiorly. Look at the area anterior and superior to the heart. This should be black, because it contains aerated lung.
- Similarly the area posterior to the heart should be black right down to the hemidiaphragms.
- The blackness in these two areas should be equivalent; therefore you can compare one with the other. If the area anterior and superior to the heart is opacified, suspect disease in the anterior mediastinum or upper lobes.
- If the area posterior to the heart is opacified suspect collapse or consolidation in the lower lobes
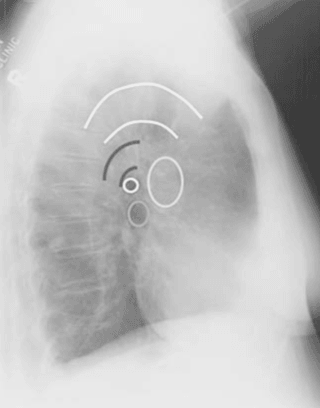
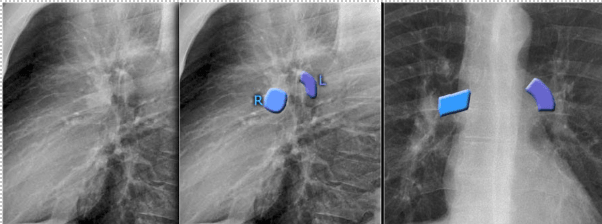
- The left main pulmonary artery (in purple) passes over the left main bronchus and is higher than the right pulmonary artery (in blue) which passes in front of the right main bronchus.
- Once you know how the normal hilar structures look like on a lateral view, it is easier to detect abnormalities.
- In this case on the PA-view there is hilar enlargement.
On the PA-view it is not clear whether this is due to dilated vessels or enlarged lymph nodes.
On the lateral view there are round structures in areas where you don't expect any vessels. So we can conclude that we are dealing with enlarged lymph nodes. - This patient has sarcoidosis.
Notice also the widening of the paratracheal line (or stripe) as a result of enlarged lymph nodes.
- On the lateral view spondylosis may mimick a lung mass.
- Any density in the area of the vertebral bodies should lead you to the PA-film to look for spondylosis, which is usually located on the right side (arrows).
On the left side the formation of osteophytes is hampered by the pulsations of the aorta.
- On the PA-view the superior mediastinum is widened.
The lateral view is helpful in this case because it demonstrates a density in the retrosternal space.
Now the differential diagnosis is limited to a mass in the anterior mediastinum (4 T's). - This was a Hodgkin's lymphoma
- A common incidental finding in adults is a Bochdalek hernia, which is due to a congenital defect in the posterior diaphragm (arrows).
In most cases, it only contains retroperitoneal fat and is asymptomatic, but occasionally it may contain abdominal organs. - Large hernias are sometimes seen in neonates and can be complicated by pulmonary hypoplasia.
- A hernia of Morgagni is also a congenital diaphragmatic hernia, but is less common.
It is located anteriorly.
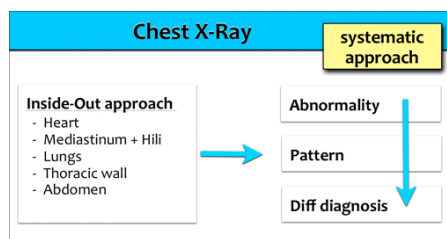
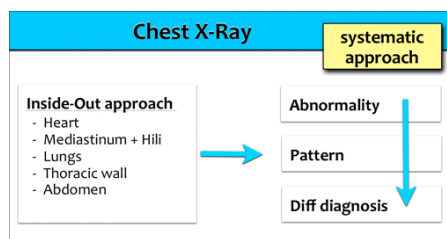
Systematic Approach
- Whenever you review a chest x-ray, always use a systematic approach.
We use an inside-out approach from central to peripheral.
First the heart figure is evaluated, followed by mediastinum and hili.
Subsequently the lungs, lung borders and finally the chest wall and abdomen are examined. - You have to know the normal anatomy and variants.
Find subtle abnormalities by using the sihouette sign and mediastinal lines.
Once you see an abnormality use a pattern approach to come up with the most likely diagnosis and differential diagnosis.
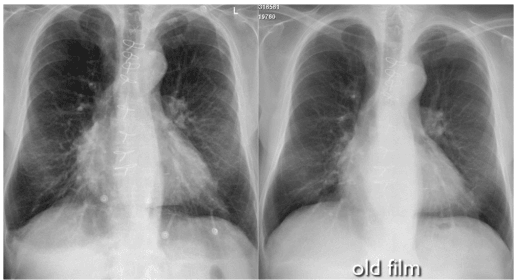
- Old films: It is extremely important to always compare with old films, as we will demonstrate in this case.
Actually, someone said that the most important radiograph is the old film, since it gives you so much information.
For instance a lung mass, which hasn't changed in many years, is not a lung cancer.
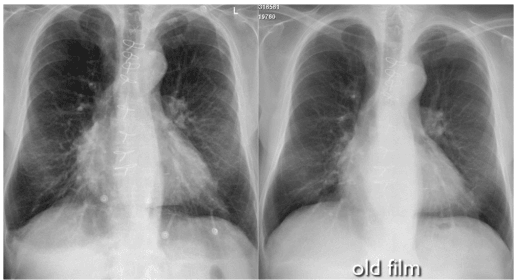
- Congestive heart failure. compared to the old film, things become more obvious and you will be much more confident in your diagnosis:
- The size of the heart is slightly increased compared to the old film.
- The pulmonary vessels are slightly increased in diameter indicating increased pulmonary pressure.
- There are subtle interstitial markings as a result of interstitial edema.
- There is pleural fluid bilaterally. Notice that the inferior border of the lower lobes has changed in position.
- All these findings indicate the presence of heart failure.
Abnormal Chest Xray
تم إنشاء هذا الموقع باستخدام Strikingly